In 2016, I got married and decided to leave my employment to start my own company alongside my new wife. After years of working in multiple sectors of the cannabis industry, I had a desire to strike off on my own as a free agent. With a highly-skilled designer by my side, it seemed like a no-brainer to combine powers into running a cannabis-focused design firm with a strong R&D component. We designed auxiliary products for the cannabis industry, created packaging, and helped launch some really cool brands. It was fun.
Not having a boss was great but being an early-stage entrepreneur seldomly results in the steady pay that one would hope for. Then the client load became unbearable—not only in the sense that I was overworked and not getting paid enough for my efforts, but also because many of the companies I was helping did not share my values and disregarded my advice on key issues that were important to me.
One of the clients during my stint running that design company was a product manufacturer who was paying me to train medical dispensaries. At the time, there were no federally regulated dispensaries. All grey market dispensaries were operating on the guise of being ‘medical compassion clubs.’ My mandate was to train retailers to take their job seriously as an important source of medicine for legitimate patients and therapeutic users, to encourage product testing, and to provide basic tips on how to help consumers stay safe.
Fortunately, this client—who shall remain nameless—strongly shared my values and allowed me to conduct this program as an important part of their community engagement initiatives. As I watched how organizations took in what they learned at my training sessions and transformed their retail and product intake process, I could not describe the pride that I felt.
The experience of working for this client left me with a great feeling for what could be accomplished when ethics and business objectives align.
During those years, I learned that one of the key issues was over-confidence. Dispelling nonsense about guiding folks purely based on flawed notions on the unanimous effects of ‘Indica’ and ‘Sativa’ was always a fun starting place. In essence, I was undoing the ‘educational efforts’ of organizations with much larger budgets and much broader reach. It sounds weird now, but back then teaching budtenders that they are not medical practitioners—and explaining how to avoid acting or speaking as such while still being able to impart useful product guidance—was in fact a groundbreaking practice in the context of the year 2014.
One of my points of focus was to teach people how to contextualize their advice as coming from a more experienced friend or host rather than from a certified health care provider. This is done kind of like the way a wine sommelier facilitates the wine-drinking experience.
The techniques I taught were very basic and focused on contextualizing information correctly and arming people with basic knowledge: the cannabinoid ratio and dose needed in order to make sensible decisions in selecting products for themselves. Keep in mind that, at the time, there were very few doctors that would or could provide even the most basic advice about how to use cannabis safely. Budtenders were literally the last line of defense and mistakes were being made. Big ones. Especially when it comes to high-risk clients.
What is a high-risk client? Well, a client who faces a condition that is known to have adverse reactions to cannabis or particular types of cannabinoids.
I can still recall the first time I worked with a client with epilepsy. The learning curve was a hard one and it included witnessing a client having a seizure in my shop due to consuming too much THC without sufficient CBD. Many years later, I also met several adults with epilepsy that also reacted poorly to long-term consumption of CBD without sufficient THC.
My role in the dispensaries I worked at was that of a front line worker and, eventually, I was put in charge of both education and data collection. Over the years, I learned—first-hand and many times over—the miracles that this plant can produce in some people while producing adverse effects/experiences in others. The patterns found in patient reports were oftentimes quite obvious and patients were actively sharing these observations with each other in person and on online blogs. Budtenders were bearing witness to an enormous amount of data but few were collecting and processing, much less doing anything about it.
I started to write down the most important observations that seemed key to helping patients find positive outcomes. I, then, cross-checked my findings with colleagues operating across Canada and in the US. The final document was the culmination of years of fieldwork helping patients gain dignified access to this plant. It was published in the form of a card set created as part of my wife’s dissertation, as she was completing her Masters in Design. I would have never finished it without her talent and constant support.
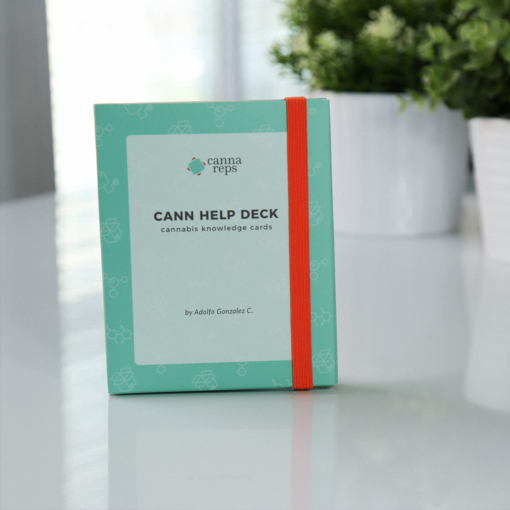
This card set became the foundation for the launch of our new company, CannaReps.
CannaReps was the culmination of all my years of training dispensary workers. I knew I loved the work and I knew it was needed. My students often came back to me telling me how impactful the training was and how it helped so many medical patients.
Looking back, I realize that constant laboratory testing of the product I was purveying was the key to broadening my understanding of this plant, how it can be used and how to help people consume it safely. It gave me eyes, while most of my colleagues operating in this rogue industry were driving blind. The matter of safety is of particular concern when it comes to high-risk patients, and my main objective was to help these people receive better guidance and avoid major pitfalls.
What pitfalls you may ask? Well, we can return to the case of clients with epilepsy—who would get told by Leafly that high-THC sativas are a good idea to try on their first swing at using the medicine to AVOID seizures. Well, as you can imagine, that was no fun for them. Pure CBD, conversely, did not seem to help adult epileptics to avoid seizures as quickly and effectively as smoking or vapourizing a cultivar with at least 2% THC and higher amounts of CBD right before the seizure onset. In fact, long-term use of purified CBD actually worsened the condition for several of my clients, with a quick recovery clearly observable upon the re-introduction of trace amounts of THC in their regimen.
Children with epilepsy on the other hand, would reportedly react rather adversely to anything above a ratio of 20:1 (CBD to THC) unless it was a particularly resistant form of epilepsy. However, if THC was completely gone from the equation (for example if isolated CBD was consumed), efficacy would decrease dramatically and much higher dosages would have to be administered to see any improvement. This modulatory interaction between THC and CBD— even at trace amounts—was obviously playing a key role in providing efficacy to this group of clients. At the time, using full-profile medicine containing both THC and CBD was not the trend amongst clinicians, who would publish studies with dosages of isolated CBD at 100mg+ in order to see meager improvements. In contrast, we were observing substantial reductions in the frequency of seizures in a great majority of our clients. Like this, we found many clear patterns in patient reports that would make any researcher say: ‘Hey, we may not have the double-blind clinical model trials to prove this, but this information will probably be useful.’ This was the difficult position I was in.
Statistical correlation does not prove causation, but there is such a thing as common sense and basic human compassion. With the information that I learned and shared with my epileptic clients, I helped hundreds of individuals and families obtain positive outcomes. I did not tell my clients that the medicine would work; nor did I represent other patients’ reports as scientifically verified data. However, I did steer patients with high-risk conditions away from high-risk products.
Learning to stay grounded in scientific thinking, while dealing with guidance information that is not scientifically verified, is a fine dance which must be learned from an experienced guide. In the case of the epileptic community, I started working with these folks around 2005 in the Downtown East Side of Vancouver. I published my first card set in 2017. I learned this dance the hard way. I thought that if my company could help people avoid knocking their heads against the wall, that this could not only improve service but perhaps even save lives.
Allow me to illustrate. When it comes to serving an epileptic, the dance would have gone somewhat like this:
Client: Hello, I am new to cannabis and I have epilepsy. Do you know what I should be taking?
Budtender: Well, I can’t tell you what will work for you, but I can tell you what other patients with your condition have reported as working. Keep in mind that these are self-reports provided to my organization and other colleagues.
Client: I understand.
Budtender: Though most of the research on people with epilepsy has been done using purified CBD in edible form which was noted to have some level of efficacy, most epileptic patients at our shop tend to use smoked or vaporized cannabis containing both THC and CBD as a form of derailing seizures before they occur. The reason being is that the effects of cannabis are felt a lot quicker when inhaled, whereas taking an edible you have to wait a couple of hours for it to take effect.
Client: Yes, when I was a child, seizures would come out of nowhere, but nowadays I can feel them coming.
Budtender: Yes, we hear all the time that this is precisely the moment when epileptic clients have reported the greatest success using cannabis. As soon as they can feel a seizure coming, they will quickly smoke or vapourize cannabis to keep the seizure at bay. Some also choose to microdose edible cannabis throughout the day, but honestly smoking and vaping seems to be the go-to.
Keep in mind that we have also heard that when epileptic clients use cannabis recreationally, it can come with risks of decreasing the efficacy of this method because their tolerance to cannabis has increased. Again, this is not scientifically verified information, but this is what clients are reporting. So, I would suggest that you remember to try to only use as much as you need to make the feeling of seizure onset go away.
Client: Which strains work best for epilepsy?
Budtender: Based on the preliminary research and feedback from other adults with epilepsy, we have found that a mixed ratio of THC and CBD works well, with CBD dominant ratios being commonly favored by more inexperienced users.
Client: Sounds good. I will try that 1:1 Harlequin.
Budtender: That is a good choice but also consider that this Cannatonic is 4:1 (CBD to THC) and is perhaps even safer for a new cannabis user. Keep in mind that the Harlequin still contains 9% THC and could produce seizures in those with high sensitivities to this compound. Also, please remember to start low and go slow, which in this case would mean to take a couple of puffs and wait before smoking the whole joint on your own. Remember that this information is anecdotal, so make sure to keep your doctor informed as to your use of cannabis and how it is affecting your reliance on any medications that you may have been prescribed.
So, this is what it was like back then. Yes, the interaction above is idealized, but that is how a properly trained person would do their job in an age where many patients were ahead of doctors in terms of their understanding of how to use this plant for their ailment.
This type of largely anecdotal information helped to improve outcomes and, in some cases, even save lives time and time again. Without doctors willing to help, it was up to experienced cannabis product vendors and a limited number of rogue researchers to provide whatever help we could. For us, seeing the effects of this plant first-hand only provided further encouragement to record and vocalize the shared experiences of clients.
Learning to share these stories as nothing more and nothing less than that: patient stories—stories that could help us live better today, not tomorrow—was for many a god-send. Yet, there are some who would call me a monster for helping an epileptic or cancer patient gain access to cannabis because “we just don’t know enough.”

Today, there are many doctors who still do not know that THC is a necessary component in medications that seek to maximize the antiseizure effects of cannabis—particularly for adults and, surprisingly, even in children. Even though pieces of data are starting to show up here and there in different studies, how long will it take for this type of knowledge to reach a medical school’s curriculum? And how long will it take to train doctors who are no longer even in medical school anymore? I always wanted to share my stories working with cancer patients, epileptics, folks in palliative care, dementia, and a whole host of conditions to anyone that would hear. I knew that the success rates we were observing were far better than those being currently achieved by the medical community for various specific conditions. However, I also knew that I had to hold back in terms of managing people’s expectations and ensuring that we were not breeding false hope. This was a fine balancing act which I engaged in as best I could for the first year running Cannareps’ Therapeutic Guidance program.
That is until the year 2018, when the Government of Canada unveiled its dispensary regulations which indicated clearly that there would be no such thing as a regulated medical dispensary. This came with good and bad sides. The bad sides are painfully obvious and already well known/felt by anyone who is a patient in this country. Basically, taking away medical dispensaries meant that patients could not talk to a budtender anymore, instead ordering cannabis online or over the phone directly with a licensed producer (LP). This created a system where those who did not grow for themselves would suffer higher prices, a complete lack of often-vital personal interaction, and less options in product diversity. This was not good.
By this time, I had been joined by my new business partner, Julie Domingo, who had been a manager for one of the dispensaries that I helped to train in Vancouver. Julie and I were left with the tasks of finding the bright side of this change and reshaping our company to continue to help cannabis vendors do a better job serving the public. This meant taking out all therapeutic guidance information and replacing it with guidance based on learning to appreciate a plant’s lineage of decent, biochemical content, and method of growing. From these changes emerged the first iteration of the Cannabis Sommelier program, which my company is known for today.
People often complain to me, saying that they used to get better service, product, and guidance from their old ‘medical’ dispensary. It is true that though there were some cases—like the Victoria Buyers Club and the BC Compassion Club—that were real ‘medical’ dispensaries that were exceptionally well-trained at providing assistance to patients, this was never the bulk of the people out there doing this work. Most paraded as ‘medical dispensaries’ while providing no special training to their staff or specialized patient-oriented services to the public. This left a bad impression on regulators and, I have to say that from a personal standpoint, I can see how some of these changes—despite representing some losses from the patient perspective—will be a win for these very same patients in the long run. Legality will allow hundreds of studies to be conducted every year which will back up many of the types of teachings that we were already working with. Because of these changes, doctors are now in the hot seat and they actually HAVE to learn to provide these services. No more scuttling under the rug to avoid this responsibility. To tell you the truth, I never felt comfortable being that person but I did because I had to. At least now, it seems like we are moving towards a better tomorrow—although there have been missteps and not just a few.
However, things will only get better if governments actually listen to the experiences of patients and react with appropriate legislative solutions. Far from eradicating the legal separation between medical and recreational users, the government should be actively funding specialized access programs for patients and providing approval and resources for cannabis research that is not purely focused on the development of patented drugs. Researchers studying full profile cannabis formats like flower and extracts must receive funding to run and share these studies as a point of public service, because this is how most people are finding efficacy in the real world. Approved drugs like Sativex and Nabilone have proven to be pricey and highly ineffective when compared to more natural forms of this medicine, so we must learn to use plants as medicine despite the complexity in running these models. There is a lot of change that needs to be made, and turning away from the plight of the patient will never be the right solution.
Today, if a medical client walks into your dispensary, do not just turn them away. Learn to be compassionate—even in these times where compassion seems to have taken a back seat to business. Let the patient know that you can’t serve them and why, and do this with heart. I would recommend the conversation to go something like this:
Client: Hi, I heard cannabis can help treat my cancer and I am hoping you can help me find something suitable.
Cannabis Retail Worker: I am really sorry to hear about your medical condition. I cannot imagine the difficulty that you and your family must be going through. There are potential medical benefits to using cannabis, but I am sorry to say that I do not have the training or medical background to truly understand your condition and medical history, and I am required by law to avoid providing this type of consumer guidance.
Client: Well, that is very disappointing. I know cannabis helped my friend with cancer, and she goes to the dispensary all the time.
Cannabis Retail Worker: I would love to help and can understand your frustration, but I simply cannot. The protocol recommended by Health Canada, the medical community, and this store is for you to first discuss with your doctor about your interest in using cannabis, and receive your cannabis via the mail from a Licensed Producer. Your doctor will be much more well-equipped to provide you guidance and monitor your health. Oftentimes there are interactions between cannabinoids (which are the medically active components of the plant) and other pharmaceutical drugs.
Client: But my doctor is very conservative and I’m afraid to bring this up to him.
Cannabis Retail Worker: Many doctors, especially the more traditional type, can be less open to discussing cannabis treatments. If you are still finding resistance from your doctor, I can refer you to some cannabis-friendly medical clinics that can take care of you. Would you like a referral?
Client: Sure.
Cannabis Retail Worker: Here you go! For future reference, keep in mind that under the current regulations, it is only “recreational users” that can be served out of stores like this. “Medical users” must acquire their cannabis from a Licensed Producer. This means that you must order your cannabis prescription over the phone or online and the product gets shipped to your home. Right now, there is no legal way that a medical user can come into a store to pick up their cannabis prescription. The line between “recreational” and “medical” can be blurry at times, but to be compliant to the law, we have to defer medical conversations to the medical community, and only serve customers that do not bring up their medical needs.
Client: Wow, that is very inconvenient.
Cannabis Retail Worker: It may be so, but at this moment in time, the laws were built with the intention to protect you from uninformed and unsafe product guidance. Something I encourage you to do since you are here, is to learn about cannabis, look at all the different cultivars, and SMELL them. Note down some names that pique your interest in terms of the appeal of the smell, as this may be a good guide in terms of what supplier you and your doctor may choose. Usually, people enjoy the cultivars that smell best to them. Some people prefer not to smoke or inhale cannabis, and they can ingest it, too. We can talk briefly about the onset and duration of these consumption methods, but when it comes to which product and how much to consume, it’s best to wait to talk to your doctor first. Please feel free to explore the store and come back to me when you have any non-medical related questions.
MORE FROM THE BLOG




WAIVER & RELEASE (the “Release”)
This event is conducted by CannaReps Consulting Ltd. (“CannaReps or Company”). Please read and submit below.
I am an attendee at an event hosted by CannaReps (the “Workshop“). I release CannaReps from any and all liability, claims, demands, actions and causes of action whatsoever arising out of or related to any loss, damage or injury, including death, that may be sustained by me while participating in the Workshop.
I understand and agree that:
CONFIDENTIALITY
Any confidential or proprietary information or material relating to the Company’s operations or business which I obtain from the Company or its officers, employees, agents, suppliers or customers or otherwise by virtue of my participation with the Company or by the Company’s predecessor. Confidential or proprietary information or material includes, without limitation, the following types of information or material, both existing and contemplated, regarding the Company or its parent, affiliated or subsidiary companies: corporate information, including contractual licensing arrangements, plans, strategies, tactic, policies, resolutions, patents, trademarks, printed or digitized materials, handouts and brochures. Including any marketing information including sales, investment and product plans, customer lists, strategies, methods, customers, prospects and market research data. Including trade secrets; technical information, including drawings, designs, personal information (the “Confidential Information”).
I understand that the copyright and proprietary interest of any material provided to me belongs to CannaReps. All shared experiences from the Workshop are to remain confidential and private. I agree not to disclose any of the information learned during the Workshop outside of the Workshop except with others who attend the Workshop. I will not use any audio or video recording equipment during the Workshop, unless CannaReps approves of the recording and filming by providing prior written consent. I understand that any audio or video recording made during the Workshop is the property of CannaReps. I will not use CannaReps’ information for business or commercial purposes, without first obtaining the prior written consent of CannaReps.
INTELLECTUAL PROPERTY
I understand, acknowledge and agree that all copyright, trademarks, trade secrets, intellectual property rights, and any other rights arising from any designs, and all of the work products and materials conceived, developed or created by the CannaReps and any rights ancillary thereto (collectively, “Intellectual Property Rights”) which were solely or jointly with others, conceives, designs, creates, derives, develops or makes in the course of or in connection with the work with CannaReps shall belong solely to CannaReps. If you haven’t already, you shall promptly disclose to CannaReps in writing any and all Intellectual Property Rights, conceived, created, derived, developed or made in the course of or otherwise in connection with my participation with CannaReps, whether alone or with others, and whether during work shop hours or through the use of facilities and properties of CannaReps.
INDEMNITY
I agrees to indemnify and hold harmless CannaReps, its officers and directors, employees and its affiliates and their respective successors and assigns and each other person, if any, who controls any thereof, against any loss, liability, claim, damage and expense whatsoever (including, but not limited to, any and all expenses whatsoever reasonably incurred in investigating, preparing or defending against any litigation commenced or threatened or any claim whatsoever) arising out of or based upon any false representation or warranty or breach or failure by me to comply with any covenant or agreement made by me herein or in any other document furnished by me to any of the foregoing in connection with this transaction.
CONSENT
Notwithstanding the immediately preceding paragraph, I consent to and grant CannaReps, the Workshop, and its assignees, the right to photograph and record me, my name, voice, appearance and likeness and other material furnished by me for use on trusted online media which include, but are not limited to, their website and social media pages. My hereby release said matter in perpetuity to CannaReps without prejudice and acknowledge that this consent is freely given without expecting compensation.
By submitting my email address below, I agree to receive electronic communication from CannaReps including personal course information, news, updates and promotions regarding CannaReps’ products. I understand that I can withdraw my consent at any time.
PRIVACY POLICY
Protecting your privacy is important to CannaReps. This Privacy Policy (“Privacy Policy”) set outs the ways in which we use your information and how we ensure its protection.
CannaReps will only collect personal information (“Information”) that will allow us to provide, enhance, market or improve our events and services. Information is collected by means of registration for any CannaReps sponsored event or service. Information collected may include name, age, gender, address, email address, payment information, and geographical information.
CannaReps may share Information. CannaReps retains the right to share Information and other statistics with our partners, prospective advertisers, and other third parties for the purposes of improving, protecting, enhancing, and promoting our events and services. CannaReps may also disclose information to our affiliates, agents, contractors, and service providers in order to facilitate the functioning and maintenance of our events and services. We will not sell any information to advertisers or other third parties.
This Privacy Policy only covers the treatment of Information and other non-identifiable information gathered by CannaReps. This Privacy Policy does not apply to the practices of any third-party services. CannaReps does not take responsibility for the content or privacy policies of any third parties. CannaReps recommends that you review the privacy policies of any third-party service providers or events you access, use, or register for through our events or services.
This Privacy Policy has been established to help you understand our commitment to protecting your privacy. CannaReps reserves the right, at any time, to change or replace any portion of our Privacy Policy. You will be notified of any changes, if we believe, they materially impact your experience at our events or services. Continued use of our services after any change to the Private Policy constitutes an acceptance of those changes.
By submitting this Release and providing Information during the registration process, including the Exhibitor’s Agreement, you consent to the collection and use of your Information for these purposes.
If you have any questions or concerns please email us at info@cannareps.ca.